Introduction
You expect menopause to bring physical changes — the hot flushes, the irregular cycles, the nights spent adjusting the duvet like it’s a stubborn piece of origami. But anxiety? The sudden rush of adrenaline in the middle of a perfectly normal afternoon, or the gnawing unease that makes you cancel plans you were once excited about? That can feel like it’s come out of nowhere.
For many women, anxiety during perimenopause and menopause is one of the most destabilising symptoms. It can be subtle — a background hum of worry — or intense, with physical sensations like a racing heart, tight chest, or trembling hands. What makes it particularly challenging is how it can sneak into daily life, changing how you feel about work, socialising, and even your own resilience. Left unaddressed, it can chip away at your confidence and quality of life.
But here’s the part too often missed in the conversation: this isn’t “just stress” or a sign you’re not coping. It’s a physiological response to hormonal changes that affect brain chemistry, stress regulation, and mood. The good news? Once you understand why it happens, there are proven, practical strategies — from medical treatments to lifestyle shifts — that can ease symptoms and help you feel more like yourself again.
Let’s start by understanding exactly what menopause anxiety is — and how to recognise it when it shows up.
Understanding Anxiety During Menopause
Menopause anxiety isn’t always the first thing people expect when they picture this stage of life. Hot flushes, yes. Irregular cycles, sure. But lying in bed at 2:17am, heart racing as if you’ve just been asked to give an impromptu TED Talk? That part often catches women off guard. This section explores why anxiety can suddenly feel sharper during perimenopause and menopause – and what’s going on inside your body and mind.
What Menopause Anxiety Feels Like
-
Persistent, low-level unease that seems to have no clear cause – the “hum” of worry in the background.
-
Sudden surges of panic, sometimes mistaken for heart problems.
-
Physical sensations: rapid heartbeat, shallow breathing, sweating at the wrong moments.
-
Emotional shifts: irritability, dread, and a sense you can’t quite trust your own reactions.
-
Overlap with generalised anxiety disorder, which can make diagnosis tricky without looking at hormonal context.
The Science: Hormones and the Brain
-
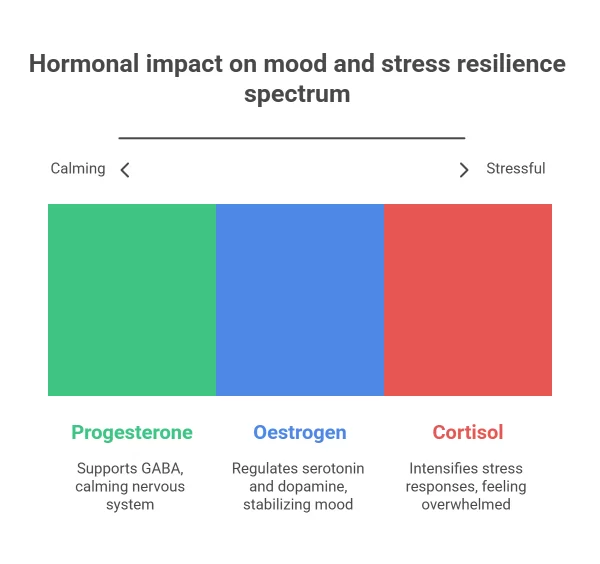
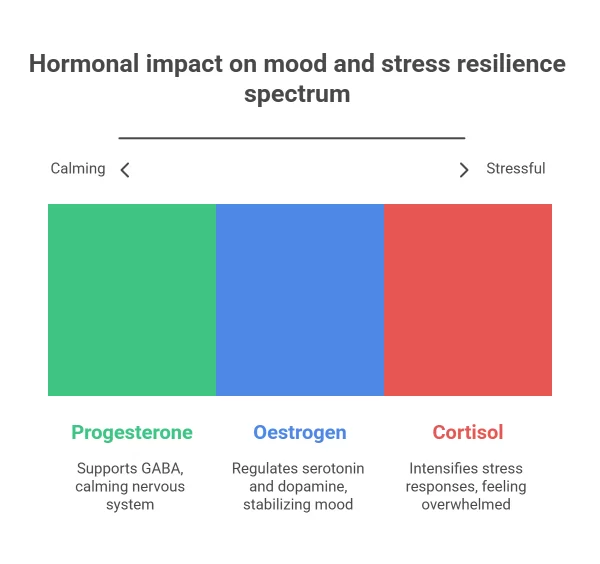
Oestrogen and neurotransmitters: Oestrogen helps regulate serotonin and dopamine, both key to mood stability. As levels drop, so can your resilience to stress.
-
Progesterone and GABA: Progesterone supports GABA, the brain’s natural calming chemical. Lower levels may mean your nervous system stays on “high alert” longer.
-
Cortisol changes: Hormonal fluctuation can make stress responses more intense – the same situation might feel more overwhelming than it did ten years ago.
-
Why timing matters: Perimenopause can involve rapid hormonal shifts, so symptoms can spike unpredictably rather than steadily.
Menopause-related anxiety isn’t imagined, overblown, or “just stress”. It’s rooted in very real changes to brain chemistry and the body’s stress response system. Understanding the biology can be the first step in reclaiming a sense of control.
If you’re starting to recognise these patterns in yourself, you might find our guide to managing menopause anxiety helpful, with practical steps and treatment options discussed in depth.
The Emotional Impact and Daily Life
Anxiety during menopause isn’t just an internal experience – it can quietly (or sometimes loudly) seep into everyday life. A morning meeting that used to be routine now feels like a performance under a spotlight. A simple dinner with friends can spark an irrational worry you’ll say something odd or forget the thread of the conversation. These moments add up, and they change how you show up in the world.
How Anxiety Affects Work and Professional Identity
-
Confidence dips: Even seasoned professionals can feel like imposters when brain fog or anxious tension takes over mid-presentation.
-
Productivity shifts: Tasks take longer when your mind is juggling intrusive thoughts alongside actual to-do lists.
-
Workplace stigma: Menopause is still poorly discussed in some industries, leading many women to mask symptoms rather than seek accommodations.
-
Career decisions: Anxiety can influence whether someone goes for a promotion or opts to step back from leadership roles.
How It Shapes Relationships and Social Life
-
Irritability and withdrawal: You might snap at loved ones or start avoiding social plans, not because you’ve stopped caring, but because the mental load feels too heavy.
-
Misunderstandings: Partners or friends may see mood changes as personal rather than physiological, straining connections.
-
Loss of spontaneity: Even enjoyable events require more emotional preparation, reducing those carefree “why not?” moments.
-
Loneliness creep: Skipping enough social invitations can create a gap that’s harder to close later.
When anxiety begins to influence the choices you make at work or in relationships, it’s more than just a passing mood. Recognising this pattern is a sign it’s worth addressing – not a sign you’re failing to cope.
Explore our evidence-based strategies for managing menopause-related anxiety to help restore confidence at work and connection in your relationships.
Myths, Misconceptions, and What No One Tells You
One of the hardest parts about menopause anxiety is how often it’s misunderstood – sometimes even by healthcare providers. Well-meaning friends may say “it’s just stress” or “it’ll all stop once your periods end” without realising how layered and unpredictable the reality can be. Let’s unpack the most common myths so you can spot them, challenge them, and avoid the guilt or confusion they tend to cause.
Myth 1: “It’s Just Stress”
-
Why it’s misleading: Stress and anxiety share symptoms like racing thoughts and rapid heartbeat, but menopause anxiety has a distinct hormonal driver.
-
The risk of mislabelling: If it’s assumed to be purely stress-related, you may miss out on treatments like HRT or menopause-specific CBT.
-
A better way to view it: Stress may be a trigger, but fluctuating hormones change how your body reacts to it – making everyday challenges feel magnified.
Myth 2: “It Ends Overnight”
-
Reality check: Anxiety often improves after hormone levels stabilise post-menopause, but the shift can be gradual rather than instant.
-
Post-menopause considerations: Some women continue to experience heightened anxiety if other health factors or unresolved triggers remain.
-
Why it matters: Setting realistic expectations can help reduce frustration and encourage ongoing self-care instead of waiting for a magic “end date.”
When you can separate fact from fiction, you can approach menopause anxiety with more clarity and less self-blame. Understanding what’s truly happening allows you to choose treatments and coping strategies with confidence.
If you’ve been told “it’s just stress” or are waiting for it to vanish on its own, our real-world menopause anxiety success stories may help you see new options.
Finding the Right Support
You don’t have to go through menopause anxiety on your own – though it can sometimes feel that way. The right mix of professional guidance, peer connection, and trusted resources can make a real difference in both your symptoms and your sense of control.
Professional Help in the UK
-
NHS pathways: Your GP can refer you to menopause clinics, mental health services, or prescribe relevant medication. While wait times can vary, it’s often the first step for many women.
-
Private menopause specialists: Offer tailored treatment plans, often with quicker access to hormone testing, HRT, and follow-up care.
-
Specialist anxiety clinics: Some focus on hormonal health as part of their mental health support – worth exploring if anxiety is your main concern.
-
Choosing the right provider: Look for practitioners registered with the British Menopause Society or relevant medical boards.
Peer and Community Support
-
Menopause cafés: Informal meet-ups across the UK where women share experiences without judgement.
-
Local support groups: Often run through community centres or women’s health charities.
-
Online communities: Forums and social media groups can be a lifeline for shared advice – but be selective to avoid misinformation.
-
Mentorship from women further along: Hearing “I’ve been there, and it does get better” from someone credible can be incredibly reassuring.
Finding your people – whether that’s a knowledgeable GP, a private clinic, or a circle of peers – can be the turning point between feeling adrift and feeling supported.
Browse our directory of trusted menopause specialists and support groups to take the next step towards feeling more like yourself.
Conclusion
Menopause anxiety can feel like it’s reshaping parts of your life you once took for granted – from how you show up at work to the way you connect with people you love. The science tells us it’s not “all in your head”, and the lived experiences of countless women prove it can be managed with the right combination of understanding, support, and treatment.
If there’s one thing to carry forward, it’s that you don’t have to navigate this quietly. Whether you choose to speak with a GP, explore HRT, try CBT, or simply start with a few small daily changes, each step is a signal to your mind and body that you’re taking this seriously – and that relief is possible.
Your next move doesn’t need to be dramatic. Book that consultation you’ve been considering, look up a menopause café in your area, or download a symptom tracker to start spotting patterns. What matters is beginning. And if you’d like a place to start, our guide to managing menopause anxiety is designed to give you practical tools and connect you with trusted resources, so you can feel more like yourself again.