Introduction
Menopause is supposed to bring a certain kind of closure — no more monthly cycles, no more unexpected periods ruining a white skirt or the one day you wore light linen trousers. But, for many women, that’s not quite the end of the story. Instead, months or even years later, they notice light spotting or heavier bleeding, and the uncertainty that follows can be unnerving.
This isn’t just about physical symptoms. Abnormal bleeding during menopause can unsettle even the most laid-back among us. It triggers questions you may not feel ready to ask — Is this serious? Will my doctor think I’m overreacting? That moment you first notice it, you might run through a mental list of every recent change in your body, your lifestyle, even your stress levels, wondering if one of them is to blame. It can feel like your body is breaking a promise you thought it had made.
But here’s the truth: while abnormal bleeding in menopause is relatively common and often caused by harmless changes, it can sometimes be a signal that something more serious needs attention. The difference between reassurance and regret often comes down to how quickly you act. In this guide, we’ll unpack what’s normal, what’s not, and why knowing the difference matters. You’ll also discover what to expect if you decide to see your GP, the range of possible causes, and the treatments available — all explained clearly, without the jargon.
So, what exactly counts as abnormal bleeding during menopause, and how can you tell when it’s time to act?
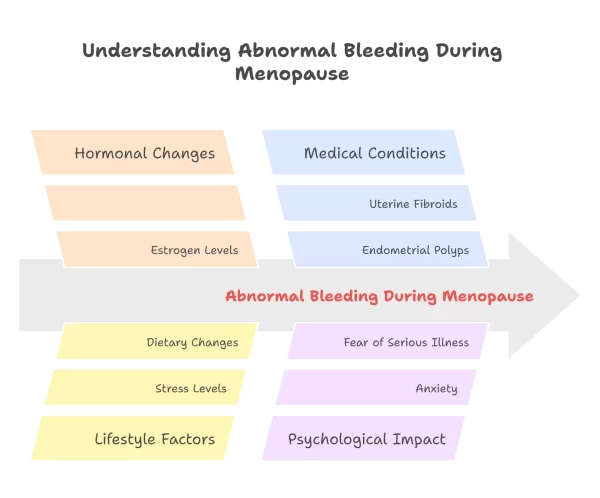
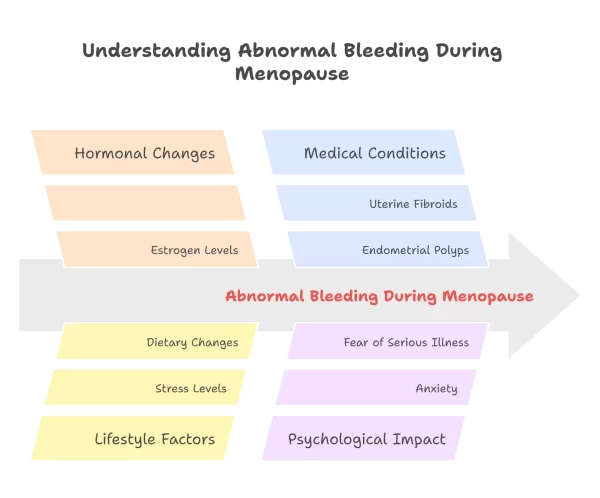
Understanding Abnormal Bleeding During Menopause
Menopause marks the end of menstrual cycles, so any unexpected bleeding during or after this stage can feel unsettling. While not every case signals something serious, understanding what is considered normal – and what is not – is the first step toward protecting your health.
Knowing the difference between peri-menopause, menopause, and post menopause
- Peri-menopause: The transition phase leading up to menopause, often marked by irregular cycles and hormonal fluctuations. This can last several years, with periods that arrive late, early, or not at all.
- Menopause: Officially reached after 12 consecutive months without a period.
- Post-menopause: The years after menopause. Any bleeding at this point is not part of a regular cycle and should be checked by a healthcare professional.
Many women notice changes like lighter spotting, sudden heavy flows, or cycles skipping months – the unpredictability can be frustrating, especially when it catches you out in light trousers on a workday.
What counts as abnormal bleeding during menopause
- Bleeding after 12 months with no periods.
- Any unexpected spotting or flow after sexual activity.
- Periods that are significantly heavier or longer than usual during the transition.
- Bleeding accompanied by pelvic pain, bloating, or fatigue.
- Even light spotting in post menopause should prompt a GP visit, as it may be linked to hormonal changes, benign growths, or – less commonly – early signs of cancer.
Recognising what is outside the spectrum of “normal” bleeding can help you seek help sooner and reduce anxiety about the unknown. Understanding your body’s patterns makes it easier to spot changes worth investigating.
Common Causes of Abnormal Bleeding
Not every episode of abnormal bleeding during menopause is cause for alarm, but some do need prompt attention. Understanding the possible reasons can help you respond with confidence instead of uncertainty.
Hormonal fluctuations in peri-menopause – the most common trigger
-
In the years before menopause, oestrogen and progesterone levels rise and fall unpredictably. This affects the thickness of the uterine lining, which can lead to heavier, lighter, or skipped periods.
-
Cycles may shorten to three weeks or stretch to two months, then surprise you with a sudden heavy flow – often on the one day you left the house without a pad or tampon.
Benign conditions – common, treatable, and still worth checking
-
Fibroids: Non-cancerous muscle growths in the uterus that may cause prolonged or heavy bleeding.
-
Polyps: Small growths on the lining of the uterus or cervix, often linked to spotting between periods or after sex.
-
Endometrial hyperplasia: Thickening of the uterine lining, sometimes related to excess oestrogen exposure.
Most of these can be detected through ultrasound or hysteroscopy and treated effectively.
More serious causes – rare but important to rule out early
-
Endometrial cancer: The most common cancer linked to postmenopausal bleeding, often diagnosed early if investigated promptly.
-
Cervical cancer: Can present as bleeding between periods or after intercourse.
-
Other reproductive tract cancers: Less common, but part of the reason any postmenopausal bleeding should be assessed.
NHS guidance is clear – any bleeding after 12 months without a period warrants medical investigation.
Knowing these potential causes is not about expecting the worst – it is about recognising patterns, ruling out serious issues, and finding peace of mind.
When to Seek Medical Advice
Some changes during menopause are expected, but specific symptoms are clear signals to see your doctor without delay. Prompt investigation not only brings peace of mind – it can make all the difference in treatment outcomes.
Red flag symptoms you should never ignore
- Bleeding after 12 consecutive months without a period.
- Heavy bleeding that soaks through pads or tampons in under an hour.
- Any bleeding after sexual intercourse.
- Bleeding accompanied by pelvic pain, bloating, or unexpected weight loss.
- Unusual vaginal discharge with a pink, brown, or blood-tinged appearance.
What to expect at a GP appointment – step-by-step clarity
- Medical history: Your doctor will ask about your menstrual patterns, symptoms, and any relevant family history.
- Physical examination: This may include a pelvic exam to check for visible changes.
- Investigations: Common first-line tests include ultrasound scans, cervical screening, and, in some cases, an endometrial biopsy.
- Referral: If further assessment is needed, you may be referred to a gynaecologist.
Most women find the process is quicker and less uncomfortable than they imagined – often likened to a smear test rather than anything invasive.
If you notice any of these symptoms, it is better to get checked and be reassured than to wait and worry. The NHS recommends prompt review of any post-menopausal bleeding, even if it happens just once.
Diagnosis and Tests
If your GP recommends further investigation, knowing what lies ahead can make the process far less daunting. Most diagnostic procedures are quick, well-tolerated, and designed to give you clear answers so that treatment – if needed – can start promptly.
Diagnostic tests – what they involve and why they matter
- Transvaginal ultrasound: A small probe is inserted into the vagina to capture detailed images of the uterus and ovaries. It helps identify changes like fibroids, polyps, or thickening of the endometrium.
- Hysteroscopy: A thin telescope-like device is passed into the uterus, allowing your doctor to view the lining directly. This may be done with or without local anaesthetic.
- Endometrial biopsy: A small sample of the uterine lining is taken for laboratory analysis, often completed in under 10 minutes.
Each test is aimed at narrowing down the cause of bleeding so treatment can be personalised.
Treatments for benign causes – targeted, effective, and often minimally invasive
- Hormone therapy: Balances oestrogen and progesterone levels to regulate or reduce bleeding.
- Minor surgical procedures: Such as polyp removal or fibroid surgery, often performed as day cases.
- Lifestyle adjustments: Weight management, dietary changes, and exercise can support hormonal balance and symptom control.
If cancer is diagnosed, clear pathways and early intervention
- Most cases of endometrial or cervical cancer detected after menopause are in the early stages, with high treatment success rates.
- Treatment plans may involve surgery, radiotherapy, or hormonal medication, tailored to your specific diagnosis.
- Support services, including counselling and specialist nurses, are available throughout treatment.
A diagnosis is the start of a plan – not the end of your options. The right combination of investigation and tailored care can resolve symptoms and protect long-term health.
Managing Emotional Impact and Next Steps
Abnormal bleeding during menopause can stir up more than just physical concerns – it can trigger anxiety, uncertainty, and that constant hum of “what if” in the back of your mind. Addressing the emotional side is just as important as managing the medical one.
Coping strategies to ease uncertainty
- Talk it through: Share your concerns with a trusted friend, family member, or support group. Sometimes just saying it out loud takes away some of its weight.
- Mindfulness and relaxation techniques: Breathing exercises, gentle yoga, or guided meditation can help calm the nervous system when health worries feel overwhelming.
- Reliable information only: Stick to trusted sources like the NHS, British Menopause Society, or Cancer Research UK to avoid spiralling into worst-case scenarios from unreliable forums.
- Keep a symptom diary: Note bleeding patterns, accompanying symptoms, and lifestyle changes – it can be surprisingly empowering to arrive at your appointment with a clear record.
Where to find ongoing support
- Specialist clinics: Menopause specialists, gynaecologists, and nurse practitioners who focus on women’s health can offer tailored guidance.
- Peer support networks: Many women find comfort in private online communities or local meet-ups where they can share experiences without judgement.
- Counselling services: Professional support can help process fear and uncertainty, especially if test results are pending.
Taking care of your emotional wellbeing during this time is not a luxury – it is a vital part of your overall health. When you feel informed and supported, you are better equipped to navigate any outcome.
Preventive Health and Monitoring
Menopause may be a natural life stage, but it is also a time when regular health checks become more critical. Staying proactive means you are more likely to catch any issues early – and feel confident about your long-term wellbeing.
Regular screenings to protect your health
- Cervical screening (smear tests): Recommended every 3–5 years in the UK, depending on age and history.
- Pelvic examinations: Allow your GP to detect changes that might not yet be causing symptoms.
- Bone density scans: Postmenopausal women are at higher risk of osteoporosis, and early detection can guide treatment.
- Annual “health MOTs”: Many women opt for a yearly package of blood tests, blood pressure checks, and physical exams to stay ahead.
Lifestyle choices that support hormonal and overall health
- Balanced nutrition: A diet rich in calcium, vitamin D, lean protein, and plenty of colourful vegetables supports both bone and cardiovascular health.
- Regular exercise: Weight-bearing activities like brisk walking or resistance training help maintain bone density and muscle strength.
- Limit alcohol and stop smoking: Both can affect hormone balance and increase the risk of certain cancers.
- Stress management: Chronic stress can disrupt sleep and exacerbate menopausal symptoms – practices like mindfulness, journaling, or even a quiet morning coffee can make a difference.
Prevention is not about living in fear of illness – it is about creating a health safety net so you can get on with life feeling strong, informed, and in control.
Conclusion
Your body’s changes during menopause are not just a medical story – they’re a personal one. Abnormal bleeding can be unsettling, but with the proper knowledge and support, it becomes something you can address with confidence rather than fear. Recognising what’s outside the “normal” range, seeking timely advice, and exploring the proper investigations are all steps towards safeguarding both your health and your peace of mind.
If there’s one thing to take away, it’s that you’re not expected to navigate this alone. Whether it’s speaking to your GP, consulting a menopause specialist, or simply starting a conversation with someone you trust, each action helps you move from uncertainty to clarity. The earlier you seek answers, the more options you have – and the more reassured you’ll feel.
If you’re ready to take the next step, consider booking a women’s health check or connecting with a reputable clinic that understands the nuances of menopause care. And if you’re not quite there yet, keep exploring reliable resources, ask questions, and stay curious about your health. Because feeling informed is not just empowering – it’s essential.